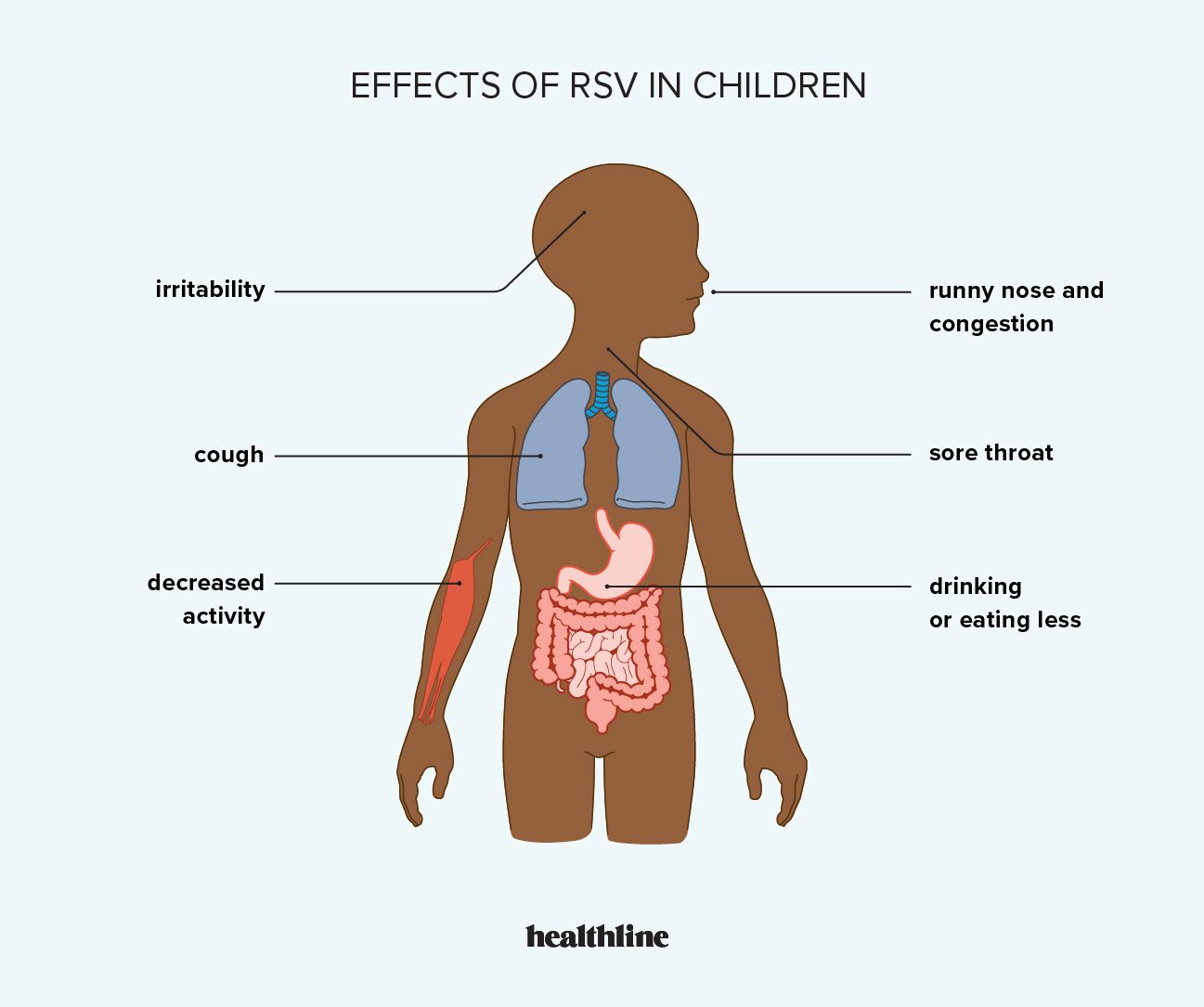
A mild cold, sore throat, and changes in appetite are common signs of RSV in children. In some cases, symptoms may be more severe.
Respiratory tract infections (RTIs) happen when an infection develops in the areas of your body that are responsible for breathing. RTIs can develop in your nose, throat, airways, or lungs.
Respiratory syncytial virus (RSV) is a common cause of RTIs in the United States. It affects approximately 5% of adults annually and is responsible for as many as
In severe cases, RSV can be life threatening. According to the National Foundation for Infectious Diseases (NFID), RSV causes an estimated 100 to 300 deaths annually in children under age 5 years.
RSV symptoms affect everyone differently, including children. Around
Among children, infants are particularly susceptible to developing severe RSV. They have smaller airways, which makes it easier for inflammation and mucus to cause obstructions. Plus, babies’ immune systems aren’t usually as strong as those of older children when it comes to fighting RSV.
Early stage
RSV can be challenging to spot in its early stage, even in infants. Symptoms may appear to be those of a mild cold. Some children may experience a fever with RSV infection.
Severe symptoms
For many children, symptoms remain mild and resolve in a few days. Some symptoms that mean RSV is progressing and medical attention is needed include:
- wheezing or difficulty breathing
- nostril flaring
- rapid, shallow breathing
- pauses in breathing, known as apnea
- blue or gray skin, lips, or nails
- prolonged or persistent vomiting
Dehydration can become a concern with RSV. Children may say they have a dry mouth or persistent thirst, for example, or they may become unable to produce tears.
Discolored urine and decreased urine output can also be a symptom of more severe RSV.
According to the
- have a neuromuscular disorder, such as those that make swallowing or clearing mucus a challenge
- were born prematurely
- are under age 12 months, particularly infants 6 months and under
- are 2 years and younger and were born with heart disease or chronic lung disease
- have a compromised immune system
Racial and ethnic disparities
RSV doesn’t discriminate. It can affect any child of any race or ethnicity, but disparities do exist.
Research from 2023 indicates that Black and Hispanic children have an increased risk of infectious respiratory diseases, such as RSV. The researchers note that several factors, such as higher rates of poverty and chronic conditions, may contribute to this increased risk.
More racial diversity in clinical trials is needed to understand why RSV disproportionately affects these communities.
Socioeconomic risk factors
Socioeconomic factors can also influence a child’s risk for RSV-related hospitalization.
The following factors can affect health outcomes for children and adults:
- limited disease education
- poverty
- language barriers
- lack of access to culturally and clinically appropriate care
A 2021 study suggested that additional socioeconomic factors that might increase a child’s RSV hospitalization risk include:
- being born to a young mother
- having a mother with involvement in the criminal system
- having a mother living with serious mental health or substance misuse challenges
- being born into a family relying on welfare-based insurance
Other vulnerable populations
Young children aren’t the only ones considered high risk for severe RSV infection. Other high risk groups include people who:
- are over the age 65 years
- have chronic heart or lung disease
- have immunosuppressive disorders or weakened immune systems
- are staying in long-term care facilities
- have underlying health conditions
Learn more about RSV in adults by visiting our resource page.
RSV affects almost all children at some point, but you can reduce the risk of exposure and help protect children who may be at risk for severe RSV.
Simple steps that can help prevent RSV include:
- avoiding close contact with people who may have RSV
- not sharing toys, bottles, cups, or utensils with others
- regularly washing hands with soap and water
- covering the mouth when sneezing or coughing
- regularly disinfecting household surfaces
- teaching children the importance of not touching their face with their hands
- not touching your child’s face with unwashed hands
Vaccination and immunization can also reduce the risk of severe symptoms.
If you’re pregnant, you can receive an RSV vaccine between weeks 32 and 36 of your pregnancy, from September through January.
If you don’t receive a vaccine, the
Monoclonal antibodies aren’t vaccines. They are products containing proteins that mimic the body’s natural antibodies to fight off infections.
RSV is a common cause of respiratory infections for both children and adults.
In children, symptoms may appear like the common cold. Coughing and congestion are typical, and fever is possible. RSV that becomes severe can cause major breathing challenges and dehydration. It can be fatal without supportive care.
Very young children, older adults, and those living with certain medical conditions are at a higher risk for severe RSV, but practical prevention steps and symptom awareness can help lower risk factors.




